Diabetic Retinopathy
If you have diabetes, you are at risk for developing diabetic retinopathy, a condition that affects the blood vessels in your eyes and can lead to vision problems. Regular eye examinations are important in the early detection of this condition.

More Diabetic Retinopathy Resources
Diabetic Retinopathy FAQ
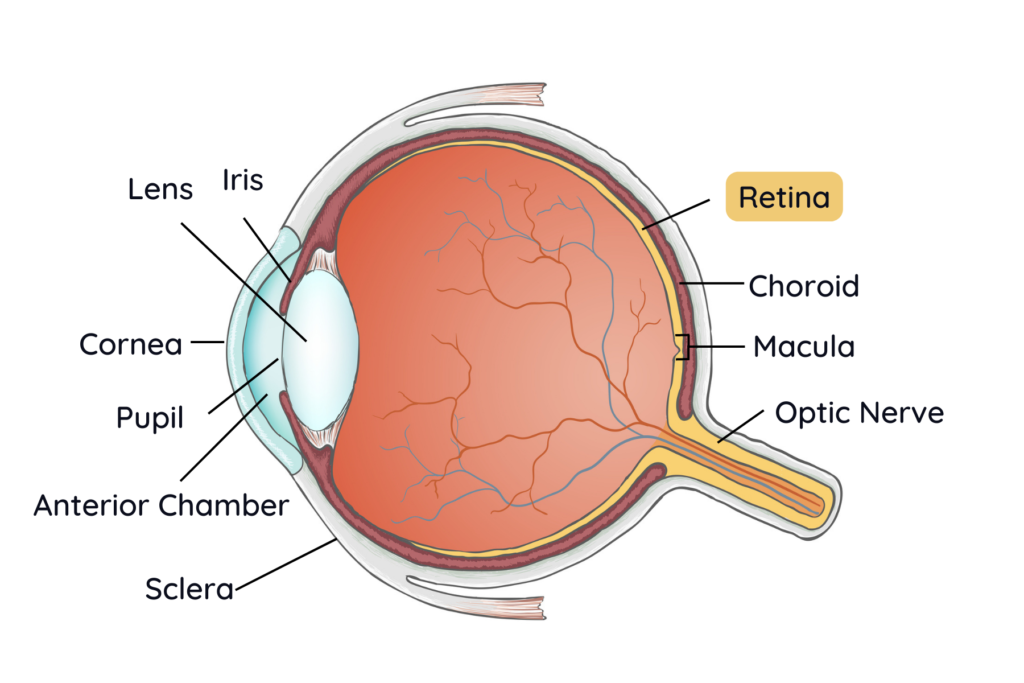
People with diabetes have trouble controlling the level of sugar in their blood. The elevated blood sugar eventually leads to a condition known as retinopathy, which refers to damage to the fine blood vessels that supply the retina. The retina is the delicate layer found in the back of your eye that functions like the film in a camera, capturing and sending visual signals to your brain from the outside world.
Damage to these blood vessels in the retina can create numerous problems such as swelling (diabetic macular edema) and bleeding. In more severe cases, the body responds to the damaged retinal blood vessels by growing abnormal new blood vessels in a process called neovascularization. Those new blood vessels are abnormal and prone to leaking, rupturing, and contraction. This can lead to blindness through conditions like retinal detachment and neovascular glaucoma.
It is typically challenging to notice the symptoms of diabetic retinopathy when the disease is in its early stages, which is why regular diabetic eye exams are very important to examine for changes in your eyes that indicate the presence of this condition. In its later stages, diabetic retinopathy can cause blurry or distorted vision, partial or total vision loss, altered color vision and floaters among other problems.
When you come in for a diabetic eye exam, your doctor uses eyedrops to dilate your pupils in order to get a better look at the inside of your eyes to evaluate for damage. Your doctor may also use special cameras to better visualize the retina and its blood vessels, such as optical coherence tomography (OCT) that takes cross-section images of your retina. These images help your doctor to assess the health your retina.
If you have Type 1 diabetes, you should have your first eye exam within five years of your diagnosis, according to the American Diabetes Association. If you have Type 2 diabetes, you should have your exam soon after your diagnosis, since Type 2 diabetes may go undiagnosed for many years.
After your first exam, you should have a diabetic eye exam once a year, or more frequently if you are at higher risk or already have more advanced forms of diabetic retinopathy. Your doctor will discuss this with you.
Like diabetes itself there is no cure for diabetic retinopathy, but it can be managed with certain treatments that slow or stop the progression of the disease. These treatments may include anti-VEGF injections, laser photocoagulation therapy and vitrectomy surgery.
Anti-VEGF medication stops the production of vascular endothelial growth factor (VEGF). This is a protein that stimulates the formation of new blood vessels. By inhibiting VEGF, abnormal blood vessels can’t form as easily and this usually slows swelling and leaking.
Laser photocoagulation treatment reduces the retina’s ability to signal for more neovascularization and can be used to close off leaking blood vessels.
Vitrectomy surgery involves removing some of the vitreous gel in the back of the eye along with scar tissue. This eases the pulling on the retina from abnormal blood vessels.
These treatments are not cures for diabetic retinopathy. Many patients need several sessions of treatment and regular monitoring to continue to prevent retinal damage. Our partnership with the expert ophthalmologists of Vitreo-Retinal Consultants Group from Wichita, Kansas allows patients to get much of their care in our Garden City clinic by these visiting physicians.
Schedule Your Visit
Our doctors are here to help address your concerns about your eyes and are experts in finding solutions that work best for you.